In partnership with our HCA Gulf Coast facilities, please see the below opportunity for 1 CNE credit on October 20, 2023.
Med Recs to Prevent Med Wrecks
Thank you,
HWS Clinical Ops Team

In partnership with our HCA Gulf Coast facilities, please see the below opportunity for 1 CNE credit on October 20, 2023.
Med Recs to Prevent Med Wrecks
Thank you,
HWS Clinical Ops Team
Topics: Gulf Coast Division, All Nurses
In partnership with our HCA Florida Lawnwood facility, please review and re-educate yourself with gastrostomy tube, continuous feeding and site care policies. We aim to ensure consistent and safe care to our patients and thank you for your partnership!
Gastrostomy, Continuous Feeding and Site Care Policies
Thank you,
HWS Clinical Ops Team
Topics: Lawnwood Regional Medical Center & Heart Institute, All Nurses, Patient Experience
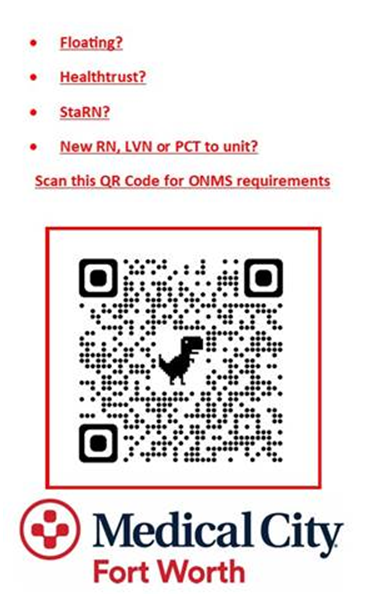
Hi HWS Team! In Partnership with our Medical City Fort Worth Ortho/Neuro Unit, please familiarize yourself with the assessment, performance and documentation requirements for post operative patients.
Please also refer to the overview sheets with QR codes that are spread throughout the unit to assist you in remembering the required assessments, performance and documentation requirements for the unit.
Thank you for your continued partnership in patient care and safety! We appreciate you!
-HWS Clinical Ops Team
Topics: Orthopedics, Patient Safety, All Nurses, Medical City Fort Worth
In partnership with our Medical City Fort Worth facility, please review the updated Suicide Huddle Card. Screening should occur in patients age 12 years and older whom are being admitted with behavioral health complaints.
Thank you for your dedication to patient safety.
HWS Clinical Ops Team
Topics: Behavioral Health, Emergency Room, Medical City, All Nurses
In partnership with our HCA Houston facilities, please review the attachment regarding higher level of care SBAR communication in rapid response situations.
Thank you for your continued commitment to patient care and safety!
Topics: All Nurses, Clear Lake Regional, HCA Houston Healthcare
In partnership with our West Florida Division facilities, please review the below attachments for Stroke Core Measure nursing education. Evidence based stroke care encompasses not only clinical aspect of the care provided, but also how well we document care provided in the medical health records. The chart audits identified an opportunity with a few areas of stroke care, such as:
Nursing units RN Stroke orientation
Discharge Stroke Education Documentation
Stroke_TIA Tips Admission and Discharge
Thank you for your dedication to patient safety!
Topics: Oak Hill Hospital, West Florida Division, All Nurses
In partnership with our facilities, please remember that texting physicians from your personal phone is not encrypted or HIPAA approved. Please see below for a refresher regarding mobile communications with physicians.
Thank you for your dedication to patient safety and HIPAA policies!
Topics: Patient Safety, San Antonio Division, All Network Staff, All Nurses
In partnership with our North Texas facilities, we are launching a new web-based application scheduling tool. Blockit is a simple web-based application that will be added to your facility’s intranet site, easily accessible from any workstation or iPad. SSO Button will automatically login users that have a profile built in Blockit based on their AD credentials. Within minutes after the ED Provider referral, staff will be able to schedule the patient’s follow up appointment at bedside.
Key Benefits
Topics: North Texas Division, Frisco, All Nurses
Within our HCA facilities, isolated events resulting in burn injury to the chest, neck, head and facial areas of the patient have been reported from defibrillator use. While defibrillator fires are not completely preventable, with appropriate precautions and techniques, the risk can be mitigated.
Please familiarize yourselves with the below documents to help us lower the risk of these events.
OR Fire Risk Assessment & Protocol
Patient Safety Defibrillator Huddle Card
Thank you for your dedication to patient safety!
Topics: Patient Safety, HCA, All Network Staff, All Nurses
In October, the North Florida Division began to transition to utilizing Plain Language Codes for activating an emergency response. This was implemented to promote standardized communication among caregivers across our NFD facilities to ensure clear communication and a coordinated response. In addition, our patients and visitors will be able to respond appropriately to events that may impact their safety.
Please see below.

Topics: North Florida Division, All Network Staff, All Nurses
As nurse leaders within HealthTrust Workforce Solutions, we partner with our colleagues to promote clinical excellence throughout the communities we serve. HealthTrust advocates on behalf of our ultimate client, the patient, ensuring that they receive the highest quality, cost-effective care in a professional, compassionate, and ethical environment.